Depsychopathologization of Gender Diversity, continued from Part 3
Kelley Winters, Ph.D.
2022 November
Depsychopathologization Policy in Early SOC Revisions
Early revisions of HBIGDA/WPATH Standards of Care more closely resembled blunt instruments of denial of medically necessary affirming care than actual standards for provision of medical care. The original SOC1 (HBIGDA, 1979, pp. 1-2) set an enduring precedent for indefinite, arbitrary deferral of affirming medical treatments, pending protracted psychological “evaluation” and assessment. “Minimal requirements” and “minimal criteria” in the SOC1 referred to lower bounds of delay for access to care, with little regard for the consequences of prolonged suffering. Health care professionals were urged to double or even triple those delays:
[Definition] 3.1 Standards of care. The Standards of care, as listed below, are minimal requirements and are not to be construed as optimal standards of care. It is recommended that professionals involved in the management of sex‐reassignment cases use the following as minimal criteria for the evaluation of their work. It should be noted that some experts on gender identity recommend that the time parameters listed below should be doubled, or tripled. (WPATH, 1979, pp. 1-2)
The SOC1 and other early versions stereotyped TGD individuals, not merely as mentally disordered, but with diminished intellect. Authors required a minimum of three months of psychotherapy before access to affirming hormonal and non-genital surgical care and six months before access to genital surgeries—whether or not there was any evidence for referral to mental health specialty care. They went so far as to recommend IQ testing, before granting access to affirming or confirming treatments.
4.3.3. Standard 3. The psychiatrist or psychologist making the recommendation in favor of hormonal and non‐genital (surgical) sex‐reassignment shall have known the patient in a psychotherapeutic relationship, for at least 3 months prior to making said recommendation. The psychiatrist or psychologist making the recommendation in favor of genital (surgical) sex‐reassignment shall have known the patient, in a psychotherapeutic relationship for at least 6 months prior to making said recommendation. That psychiatrist or psychologist should have access to the results of the psychometric testing (including IQ testing of the patient) when such testing is clinically indicated. (1979, p. 4)
Unfounded stereotypes of intrinsic TGD psychopathology and mental infirmary had enduring consequences in early HBIGDA/WPATH Standards of Care. Access to both hormonal and surgical care were further delayed by oppressive “real life experience” social role requirements (1979, p. 4). Yet more delay of affirming care was mandated for individuals with coexisting mental health conditions. This policy disallowed concurrent affirming care and mental health support and disregarded harm inflicted by denial of affirming medical care:
4.7.2. Principle 14. The patient having a psychiatric diagnosis (i.e., schizophrenia) in addition to a diagnosis or transsexualism should first be treated by procedures commonly accepted as appropriate for such non‐transsexual psychiatric diagnoses. (1979, p. 4)
Publication of the HBIGDA SOC5 and 6 (1998, 2005) brought the beginnings of critical scrutiny of these psychopathology stereotypes. A bold-font section heading in the SOC5, “The Gender Identity Disorders are Mental Disorders” (p. 16), was revised in the SOC6 to, “Are Gender Identity Disorders Mental Disorders?” (2005, p. 10). Mandatory psychotherapy requirements were dropped in the SOC5 for adults seeking affirming care:
Psychotherapy is not an absolute requirement for triadic therapy.
1. Individual programs vary to the extent that they perceive the need for psychotherapy.
2. When the mental health professional’s initial assessment leads to a recommendation for psychotherapy, the clinician should specify the goals of treatment, estimate its frequency and duration.
3. The SOC committee is wary of insistence on some minimum number of psychotherapy sessions prior to the real life experience, hormones, or surgery but expects individual programs to set these. (1998, p. 8)
Depsychopathologization Policy in the SOC 7
The WPATH Policy Statement on Depsychopathologization (2010) was prominently cited in the 7th Revision of the Standards of Care (2011B), published the following year:
Being Transsexual, Transgender, or Gender Nonconforming Is a Matter of Diversity, Not Pathology
WPATH released a statement in May 2010 urging the de-psychopathologization of gender nonconformity worldwide. This statement noted that “the expression of gender characteristics, including identities, that are not stereotypically associated with one’s assigned sex at birth is a common and culturally-diverse human phenomenon [that] should not be judged as inherently pathological or negative.” (p. 4)
The SOC7 brought forward-progress in policies that acknowledged both depsychopathologization and medical necessity principles (Winters, 2011A). These included recognition of informed consent protocols for hormonal care (WPATH, 2011, pp. 35-36), clarified guidance on puberty suppression care for gender incongruent adolescents (pp. 18-20), and removal of arbitrary delays of three months before hormonal care—pending mandatory psychotherapy or “real life experience” (p. 34).
However, the SOC7 retained barriers to care that contradicted both of WPATH’s depsychopathologication and medical necessity principles. For example, access to hormonal care and surgical procedures was obstructed unless diagnosed mental health conditions were “well controlled” (pp. 34, 59, 60, 104, 105, 106). Moreover, capricious age-of-majority restrictions on confirming surgical care (pp. 21, 60) prioritized political vagaries over medical necessity.
In many ways, the 7th Version Standard of Care did not consistently adhere to the WPATH depsychopathologization policy. However, the SOC7 brought optimism for continued progress and clarity on this principle of ethical practice by release of the SOC8.
Depsychopathologization Policy in the SOC 8
Like the SOC7, Version 8 of the WPATH Standards of Care for the Health of Transgender and Gender Diverse People (2022) fell short of clarity and closure on the principle of depsychopathologization of gender diversity and resulting barriers to affirming care. Instead, it seemed to further cloud these issues with contradiction and compromise.
Inexplicably, the WPATH Policy Statement on Depsychopathologization (2010) is not directly cited in the SOC8. It does not appear in the References section or in-text citations. Given the historical importance of this key WPATH policy on the ethical treatment of Trans and Gender Diverse individuals, this omission merits timely correction in the SOC8.
However, Chapter 2, “Global Applicability,” cites later descriptions of the depsychopathologization principle in the DSM-5 (APA, 2013A) and ICD-11 (WHO, 2019):
Mainstream global medicine no longer classifies TGD identities as a mental disorder. In the Diagnostic and Statistical Manual Version 5 (DSM-5) from the American Psychiatric Association, the diagnosis of Gender Dysphoria focuses on any distress and discomfort that accompanies being TGD, rather than on the gender identity itself…In the International Classification of Diseases, Version 11 (ICD-11)…the Gender Incongruence diagnosis is placed in a chapter on sexual health and focuses on the person’s experienced identity and any need for gender-affirming treatment that might stem from that identity. Such developments, involving a depathologization (or more precisely a de-psychopathologization) of transgender identities, are fundamentally important on a number of grounds. (WPATH, 2022, p. 15)
The principle of depsychopathologization of gender diversity is re-stated a number of times in the 8th Version, WPATH Standards of Care (2022, pp. 15, 59, 33, 117). The following table lists examples of explicit and implicit endorsements of the depsychopathologization principle in the SOC8. These include guidance that access to affirming medical care should not be withheld only because of co-occurring mental health or neuro-diverse conditions. This listing may be useful to TGD individuals, health care professionals, and affirming family members who face obstacles to care, based on false stereotypes that equate gender diversity with psychopathology:
Table 1: SOC8 Endorsements of the Depsychopathologization Principle
| SOC8 Explicit References to the Depsychopathologization Principle |
| Ch. 2, Global, p.15 Mainstream global medicine no longer classifies TGD identities as a mental disorder…developments [in the DSM-5 and ICD-11], involving a depathologization (or more precisely a de-psychopathologization) of transgender identities, are fundamentally important on a number of grounds. In the field of health care, they may have helped support a care model that emphasizes patients’ active participation in decision-making about their own health care… |
| Ch. 6, Adolescents, St. 6.12a, p. 59 The most recent versions of these two systems, the DSM-5 and the ICD-11, reflect a long history of reconceptualizing and de-psychopathologizing gender-related diagnoses… Compared with the ICD 10th edition, the gender incongruence classification was moved from the Mental Health chapter to the Conditions Related to Sexual Health chapter in the ICD-11. |
| SOC8 Implicit Endorsements of the Depsychopathologization Principle |
| Introduction, p. 7 WPATH strongly recommends against any use of reparative or conversion therapy (see statements 6.5 and 18.10). |
| Ch. 5, Adults, p. 31 Some TGD people may need a comparatively brief assessment process for GAMSTs. |
| Ch. 5, Adults, St. 5.1.c, p. 33 Gender diversity is a natural variation in people and is not inherently pathological. …The need to include an HCP with some expertise in mental health does not require the inclusion of a psychologist, psychiatrist, or social worker in each assessment. |
| Ch. 5, Adults, St. 5.1.d, p. 34 The presence of psychiatric illness or mental health symptoms do not pose a barrier to GAMSTs unless the psychiatric illness or mental health symptoms affect the TGD person’s capacity to consent to the specific treatment being requested or affect their ability to receive treatment. This is especially important because GAMSTs have been found to reduce mental health symptomatology for TGD people. |
| Ch. 5, Adults, St. 5.3.b, p. 36 There is evidence the use of rigid assessment tools for “transition readiness” may reduce access to care and are not always in the best interest of the TGD person |
| Ch. 5, Adults, St. 5.3.c, p. 37 There is no evidence to suggest a benefit of withholding GAMSTs from TGD people who have gender incongruence simply on the basis that they have a mental health or neurodevelopmental condition. |
| Ch. 5, Adults, St. 5.3.d, p. 37 Treatment for mental health problems can and should occur in conjunction with GAMSTs when medical transition is needed. It is vital gender-affirming care is not impeded unless, in some extremely rare cases, there is robust evidence that doing so is necessary to prevent significant decompensation with a risk of harm to self or others. In those cases, it is also important to consider the risks delaying GAMSTs poses to a TGD person’s mental and physical health |
| Ch. 5, Adults, St. 5.3.d, p. 37 Delaying access to GAMSTs due to the presence of mental health problems may exacerbate symptoms. |
| Ch. 6, Adolescents, p. 45 these gaps [in scientific understanding] should not leave the TGD adolescent without important and necessary care. |
| Ch. 6, Adolescents, St. 6.5, p. 53 We recommend against offering reparative and conversion therapy aimed at trying to change a person’s gender and lived gender expression to become more congruent with the sex assigned at birth. …Conversion/reparative therapy has been linked to increased anxiety, depression, suicidal ideation, suicide attempts, and health care avoidance…efforts undertaken a priori to change a person’s identity are clinically and ethically unsound. We recommend against any type of conversion or attempts to change a person’s gender identity… |
| Ch. 7, Children, p. 67 conversion therapies for gender diversity in children (i.e., any “therapeutic” attempts to compel a gender diverse child through words, actions, or both to identify with, or behave in accordance with, the gender associated with the sex assigned at birth are harmful and we repudiate their use. |
| Ch. 7, Children, St. 7.2, p. 70 Gender diversity is not a mental health disorder; (see contradictory concerns with this compound sentence in 7.2, Table 2) |
| Ch. 7, Children, St. 7.13, p. 77 not all gender diverse children wish to explore their gender. Cisgender children are not expected to undertake this exploration, and therefore attempts to force this with a gender diverse child, if not indicated or welcomed, can be experienced as pathologizing, intrusive and/or cisnormative. (see contradictory concerns with 7.13 in Table 2) |
| Ch. 12, Hormone, St. 12.8, p. 117 Providers should keep in mind being transgender or questioning one’s gender does not constitute pathology or a disorder. Therefore, individuals should not be referred for mental health treatment exclusively on the basis of a transgender identity. |
| Ch. 12, Hormone, St. 12.21, p. 126 Withholding hormone therapy based on the presence of depression or suicidality may cause harm. …the practice of withholding hormone therapy until these symptoms [of depression and anxiety] are treated with traditional psychiatry is considered to have iatrogenic effects. |
| Ch. 12, Hormone, St. 12.21, p. 127 If psychiatric treatment is indicated, it can be started or adjusted concurrently without discontinuing hormone therapy. |
| Ch. 18, Mental Health, p. 171-172 Addressing mental illness and substance use disorders is important but should not be a barrier to transition-related care. Rather, these interventions to address mental health and substance use disorders can facilitate successful outcomes from transition-related care, which can improve quality of life. |
| Ch. 18, Mental Health, St. 18.2, p. 172-173 The benefits of mental health treatments that may delay surgery should be weighed against the risks of delaying surgery and should include an assessment of the impact on the patients’ mental health delays may cause in addressing gender dysphoria. |
| Ch. 18, Mental Health, St. 18.9, p. 175 We recommend health care professionals should not make it mandatory for transgender and gender diverse people to undergo psychotherapy prior to the initiation of gender-affirming treatment, while acknowledging psychotherapy may be helpful for some transgender and gender diverse people. |
| Ch. 18, Mental Health, St. 18.10p. 176 We recommend “reparative” and “conversion” therapy aimed at trying to change a person’s gender identity and lived gender expression to become more congruent with the sex assigned at birth should not be offered. …“conversion therapy” has not been shown to be effective. In addition, there are numerous potential harms. |
Depsychopathologization Contradictions in the SOC 8
Unfortunately, endorsements and corollaries of WPATH’s depsychopathologization policy in the SOC8 are undermined, even directly contradicted, by regressive, conflicting Statements of Recommendation and supporting text. WPATH’s ambivalence on the depsychopathologization principle is harmful and politically weaponized against all TGD health care. Some examples of false stereotypes of TGD psychopathology in the SOC8 are listed in Table 2. This is not an exhaustive list, but it may be useful to TGD individuals, health care professionals, and affirming family members who face obstacles to medically necessary care, rooted in these contradictions to the WPATH depsychopathologization principle:
Table 2: SOC8 Contradictions to the Depsychopathologization Principle
| SOC8 Contradictions to Depsychopathologization Principle | Remarks |
| Ch. 5, Adults, St. 5.3.c, p. 36 Identify and exclude other possible causes of apparent gender incongruence prior to the initiation of gender-affirming treatments. | Statement 5.3.c presumes, without citation, scientifically unsupported stereotypes that gender diversity is caused by underlying mental illness. It undermines the WPATH depsychopathologization and medical necessity principles by asserting that affirming care be delayed indefinitely, pending a psychopathologized fishing expedition for behavioral “causes” of gender incongruence, with no scientific basis. Statement 5.3.c is further contradicted by its own supporting text (Table 1). |
| Ch. 5, Adults, St. 5.5, p. 40 The authors posited when clients are adequately prepared and assessed under the care of a multidisciplinary team, a second independent assessment is unnecessary. | This sentence incorrectly implies that a second, independent (comprehensive bio-psycho-social…) assessment, with consequential delay of medically necessary care, is inexplicably necessary for adults who select their own affirming health professionals, outside of a mental health specialist in a centralized “multidisciplinary team.” Ironically, it is contradicted by the immediately preceding sentence, describing “paternalism” and “potential breach of the autonomy” in health care systems (p. 40). |
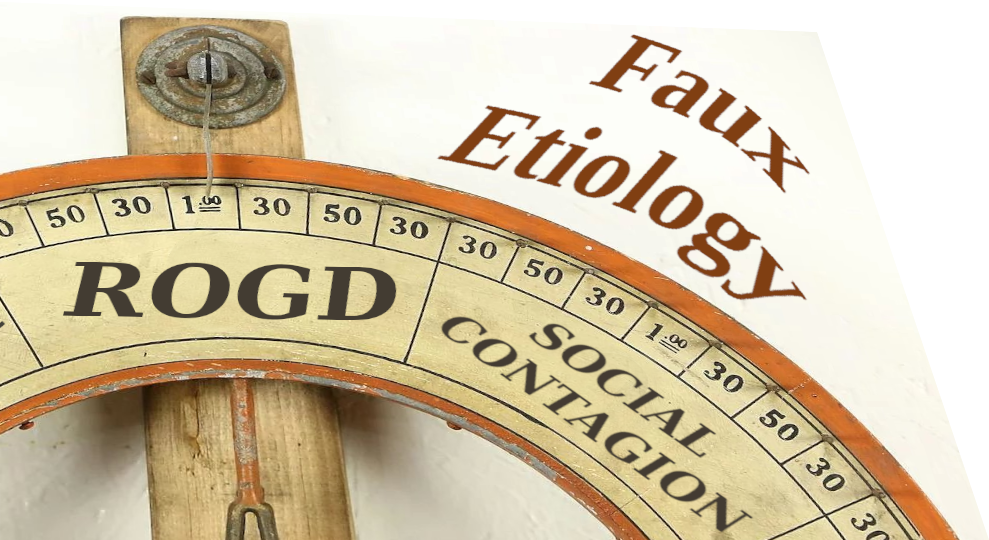
| Ch. 6, Adolescents, p. 45 For a select subgroup of young people, susceptibility to social influence impacting gender may be an important differential to consider | This sentence is an endorsement of the scientifically bankrupt “rapid-onset gender dysphoria” (ROGD) and “social contagion” myths about gender diverse youth. They spreads political panic about fictitious mental “contagion” that turns cisgender kids Trans, through social media and school groups. |
| Ch. 6, Adolescents, St. 6.3, p. 50 comprehensive biopsychosocial assessment of adolescents who present with gender identity-related concerns and seek medical/surgical transition-related care…MHPs have the most appropriate training, experience, and dedicated clinical time required to obtain the information discussed here…The assessment should occur prior to any medically necessary medical or surgical intervention under consideration (e.g., puberty blocking medication, gender-affirming hormones, surgeries). | This statement presumes inherent TGD psychopathology and is reminiscent of compulsory long-term psychotherapy requirements in the SOC1 through SOC4. It demands that medical care for all adolescents should be delayed, pending compulsory, protracted MH assessment before and not offered concurrently. Referral to specialized MH services is doctrinal for all TGD adolescents, simply because they are TGD. It contradicts guidance in the same chapter that “gaps [in understanding] should not leave the TGD adolescent without important and necessary care” (Table 1, p. 45), as well as affirming guidance on (Table 1, pp. 117, 127, and 175). |
| Ch. 6, Adolescents, St. 6.3, p. 51 There are no studies of the long-term outcomes of gender-related medical treatments for youth who have not undergone a comprehensive assessment. Treatment in this context (e.g., with limited or no assessment) has no empirical support and therefore carries the risk that the decision to start gender-affirming medical interventions may not be in the long-term best interest of the young person at that time. | This statement is a denying-the-antecedent logical fallacy, asserting a hysterical,frightening conclusion for an inverse condition, for which the authors offer no data. It presumes inherent psychopathology of all TGD youth and projects unsupported fear, to compel long-term psychotherapy that is prerequisite to affirming medical care. This contradicts guidance on p. 45 of the same chapter (Table 1). |
| Ch. 6, Adolescents, St. 6.3, p. 53 It is important to note potential factors driving a young person’s gender-related experience and report of gender incongruence, when carried out in the context of supporting an adolescent with self-discovery, is not considered reparative therapy as long as there is no a priori goal to change or promote one particular gender identity or expression. | This text presumes unsupported stereotypes that gender diversity is caused by underlying mental illness. Compulsory “gender exploration” fishing expeditions for behavioral “causes” or “etiologies” of gender incongruence are contrary to the depsychopathologization principle. Unless freely initiated and led by the TGD youth, these practices can be covertly punitive and have been proposed by disaffirming policymakers as a “loophole” to prohibitions on gender-conversion practices (Winters, 2022B). |
| Ch. 6, Adolescents, St. 6.11, p. 58 cases in which the parent(s)/caregiver(s)’ questions or concerns are particularly helpful in informing treatment decisions and plans…situations in which a young person experiences very recent or sudden self-awareness of gender diversity and a corresponding gender treatment request, or when there is concern for possible excessive peer and social media influence on a young person’s current self-gender concept. | Lacking citations, this paragraph is a back-door endorsement of the biased, flawed myths of “rapid-onset gender dysphoria”(ROGD) and “social contagion.” These are recent variations of unsupported psychopathological stereotypes of TGD youth that have been perpetuated for generations. The “ROGD” myth conflates closeted circumstance with cisgender status. It misrepresents coming out in adolescence as “rapid onset;” and it spreads political panic about fictitious mental contagion that turns cisgender kids Trans, through social media and school groups. |
| Ch. 6, Adolescents, St. 6.12b, p. 61 Critically, these findings of low regret can only currently be applied to youth who have demonstrated sustained gender incongruence and gender-related needs over time as established through a comprehensive and iterative assessment (see Statement 6.3). | This statement is a denying-the-antecedent logical fallacy, asserting a hysterical, frightening conclusion for an inverse condition. The authors offer no evidence of disproportionate detransition rates for adolescents receiving care under affirming protocols. It presumes inherent psychopathology of all TGD youth and projects unsupported fear of regret. “Iterative” long-term psychological interrogation of a TGD adolescent’s identity, in lieu of medically necessary care, contradicts guidance on p. 45 of the same chapter (Table 1). |
| Ch. 6, Adolescents, St. 6.12d, p. 62 Evidence indicates TGD adolescents are at increased risk of mental health challenges, often related to family/caregiver rejection, non-affirming community environments… A young person’s mental health challenges may impact their conceptualization of their gender development history and gender identity-related needs… | These two sentences conflate correlation with causality in a paradox—suggesting without evidence that gender diversity is caused by mental disorder, which is caused by family rejection of gender diversity, which is caused by mental disorder, and so on. This is a twisted form of the psychopathologization stereotype. |
| Ch. 7, Children, St. 7.2, p. 70 we know mental health can be adversely impacted for gender diverse children (e.g., through gender minority stress) that may benefit from exploration and support; therefore, mental health expertise is highly recommended. | This sentence psychopathologizes all gender diverse children. It casts doubt on the validity of their gender identities and calls for scrutiny (“exploration”) of their identities through psychotherapy, regardless of how consistent and stable they may be in their affirmed genders. This passage is self-contradicted within the very same compound sentence (Table 1) . |
| Ch. 7, Children, St. 7.13, p. 76 We recommend health care professionals and parents/caregivers support children to continue to explore their gender throughout the pre-pubescent years, regardless of social transition. | This statement ambiguously implies compulsory “gender exploration” psychotherapy for TGD youth, throughout prepubescent childhood. It presumes unfounded stereotypes of psychopathology and gaslights the identities of TGD children, who may be long-established and well-adjusted in their authentic social gender roles. Unless freely initiated and led by the TGD youth, these practices can be covertly punitive. 7.13 is contradicted within its own supporting text (Table 1). |
| Ch 13, Surgery, St. 13.7, p. 133 We recommend surgeons consider gender- affirming surgical interventions for eligible transgender and gender diverse adolescents when there is evidence a multidisciplinary approach that includes mental health and medical professionals has been involved in the decision-making process. | This statement demands compulsory, long-term psychotherapy that is prerequisite to access for confirming surgical care. It rests on the stereotype of intrinsic psychopathology of TGD adolescents. In some cases, a trusted, long-term medical provider, qualified in TGD care, may be better situated to perform appropriate assessment. This statement also contradicts Statement 18.2 text in the Mental Health chapter (Table 1) |
The Double Standard of Psycho-Gatekeeping of TGD Medical Care
The examples of psychopathological stereotyping of gender diversity in Table 2 are not problematic because they require diagnostic assessment. They are problematic because they single out Trans and Gender Diverse people for social stigma, compulsory long-term mental health specialty referral, and vastly disparate barriers to affirming medical and surgical care—simply because they are TGD and therefore presumed, without evidence, to be mentally ill.
Medical assessment and some form of diagnostic and billing coding are often useful to establish medical necessity and prioritization of resources in health care systems worldwide. Intake assessment in cisgender settings commonly includes psychosocial screening, with referral to specialized mental health care only when indicated by evidence. In contrast, regressive parts of the SOC8 recommend automatic referral of TGD children, adolescents, and adults to specialized mental health clinicians, simply because of gender diversity (Table 2, pp. 40, 50, 70, 133).
For example, Statement 6.3 in the Adolescents chapter of the SOC8 requires that medically necessary pubertal suppression or affirming hormonal treatment be deferred, pending completion of compulsory, long-term “comprehensive biopsychosocial assessment of adolescents who present with gender identity-related concerns” (p. 50). This is to be administered by a third-party mental health provider (p. 50), rather than a qualified medical practitioner or clinic—even if the latter might have years of prior familiarity with the patient. It further suggests invasive (and often offensive) “psychometrically validated psychosocial and gender measures” (p. 51). The latter place a further disparate burden of proof upon TGD adolescents to repeatedly demonstrate their competence and validity of their authentic selves. In contrast, adolescents of cisgender privilege would never be presumed mentally ill and denied medical care because they are cisgender. The double standard in the SOC8 is stunning, yet it is contradicted by affirming guidance within the same chapter and in the Adults and Mental Health chapters:
Some TGD people may need a comparatively brief assessment process for GAMSTs. (p. 31)
While future research will help advance scientific understanding of gender identity development, there may always be some gaps. Furthermore, given the ethics of self-determination in care, these gaps should not leave the TGD adolescent without important and necessary care. (p. 45)
There is evidence the use of rigid assessment tools for “transition readiness” may reduce access to care and are not always in the best interest of the TGD person. (p. 36)
individuals should not be referred for mental health treatment exclusively on the basis of a transgender identity. (p. 117)
We recommend health care professionals should not make it mandatory for transgender and gender diverse people to undergo psychotherapy prior to the initiation of gender-affirming treatment, while acknowledging psychotherapy may be helpful for some transgender and gender diverse people. (p. 175)
“ROGD” Hysteria and Mythical Etiologies
WPATH publicly rejected Lisa Littman’s faux diagnostic term of “Rapid-Onset Gender Dysphoria” and discouraged related psychopathologizing stereotypes that “instill fear about the possibility that an adolescent may or may not be transgender” (2018; Littman, 2018). Yet, the SOC8 supports Littman’s pseudo-science in numerous statements and inferences that gender incongruence is a manifestation of myriad mental and developmental disorders, intellectual deficiency, past trauma, and, nonsensically, social exposure to the existence of TGD human beings (pp. 36, 45, 53, 58, 62, and others). Most troubling, these assertions in the SOC8 demand that affirming medical care for adolescents and adults should be denied or delayed until long-term psychotherapy is completed to dig up assumed, psychopathological “causes” of gender incongruence. Facing a priori presumption of mental defectiveness from regressive statements and text in the SOC8, TGD adolescents and adults seeking affirming medical care must bear an unconscionable burden of proof to demonstrate their mental competence and gender identities. This contradicts both the “WPATH De-Psychopathologization Statement” (2010) and the “WPATH position on ‘Rapid Onset Gender Dysphoria’” (2018).
For example, Statement 6.11 in the Adolescents Chapter is nearly explicit in endorsing Littman’s flawed “ROGD” and “social contagion” stereotypes:
…a parent/caregiver report may provide critical context in situations in which a young person experiences very recent or sudden self-awareness of gender diversity and a corresponding gender treatment request, or when there is concern for possible excessive peer and social media influence on a young person’s current self-gender concept. (p. 58)
Lacking citations, this text conflates the closet with cisgender status, misrepresents coming out in adolescence as “rapid onset,” and spreads political panic about fictitious mental “contagion” that turns cisgender kids Trans, through social media and school affinity groups. Following Littman’s model (2018), this text centers the perceptions of “rapid onset” by disaffirming parents, rather than the lived experiences of TGD adolescents. Compulsory, long-term, psychotherapy fishing expeditions for behavioral “causes” of gender incongruence are recommended in the same chapter (p. 53), as prerequisite to gender-affirming medical care.
The stereotype of psychopathological “etiology” of gender incongruence and the mischaracterization of experienced gender incongruence as confusion are extended to adults in Statement 5.3.c. Here, compulsory psychotherapy is recommended to “identify and exclude other possible causes of apparent gender incongruence prior to the initiation of gender-affirming treatments” (p. 36).
The SOC8 editors erred by not including the “WPATH position on ‘Rapid Onset Gender Dysphoria” (2018) in its entirety from the Standards of Care. Littman’s (2018) “ROGD” and “social contagion” stereotypes and WPATH’s public response to them are introduced to the Adolescents Chapter in coded, confusing, and poorly edited language that reads more like a squabble than a medical standard. Nevertheless, this text notes some of the fundamental flaws in the “ROGD” trope:
…the findings of the [Littman] study must be considered within the context of significant methodological challenges, including 1) the study surveyed parents and not youth perspectives; and 2) recruitment included parents from community settings in which treatments for gender dysphoria are viewed with scepticism and are criticized
…these findings have not been replicated.
…caution must be taken to avoid assuming these phenomena occur prematurely in an individual adolescent while relying on information from datasets that may have been ascertained with potential sampling bias. (p. 45)
Gender Conversion and Covertly Punitive Psychotherapies
Ethical guidance to prohibit gender-conversion or gender-reparative psychotherapies was first adopted by WPATH in the SOC7:
Treatment aimed at trying to change a person’s gender identity and expression to become more congruent with sex assigned at birth has been attempted in the past without success (Gelder & Marks, 1969; Greenson, 1964), particularly in the long term (Cohen-Kettenis & Kuiper, 1984; Pauly, 1965). Such treatment is no longer considered ethical. (2011, p. 16)
The SOC8, in their current form, stop short of the SOC7 ethical prohibition of gender-conversion psychotherapies. However, they repeat recommendations against gender-conversion practice (WPATH, 2022, pp. 7, 53, 67, 176). For example, Statement 18.10 in the Mental Health chapter asserts:
We recommend “reparative” and “conversion” therapy aimed at trying to change a person’s gender identity and lived gender expression to become more congruent with the sex assigned at birth should not be offered.
…“conversion therapy” has not been shown to be effective. In addition, there are numerous potential harms. (p. 176)
However, the SOC8 fail to address deceptive strategies that have been used to circumvent professional and legal restrictions on gender-conversion psychotherapies, by labeling them as “gender exploration therapies” (Winters, 2022B). At its 2016 biennial symposium in Amsterdam, WPATH itself platformed a session by attorney and psychiatrist, Richard Green, and psychologist, Kenneth Zucker, on evasion of laws and policies which prohibited gender-conversion practices (WPATH, 2016C). They proposed a loophole to trans-protective restrictions, by suggesting that punitive gender-conversion therapies simply be relabeled as “identity exploration”:
So, I asked a lawyer the following: ‘The bill says treatment cannot seek to change the gender identity of a patient under 18 years of age but it is OK to engage in identity exploration. What’s the difference?’ The lawyer had a very detailed analysis: ‘No one the fuck knows.’ (Zucker, 2016)
Gender exploration, in its plain-language context, is a positive process of self-discovery, when freely initiated and led by the individual. All people, TGD and cisgender, explore our individual places in a gendered society throughout stages of youth, adulthood, and elderhood. However, when “gender exploration” psychotherapies on TGD children, adolescents, and adults are not consensual, but are compulsed by psycho-gatekeeping practices, they can become punitive (Ashley, 2019) and covert forms of gender-conversion (Winters, 2022B) .
The SOC8 contains troubling recommendations for long-term “gender exploration” psychotherapies for TGD children and adolescents (pp. 53, 70, 76, and others). These lack clarification to prevent unethical exploitation of the Green-Zucker loophole to obfuscate punitive or gender-conversion psychotherapies. Compulsory “gender exploration” therapies in the SOC8 are combined with myths and stereotypes that gender incongruence is “caused” by underlying mental illness. For example, Statement 6.3 in the Adolescents chapter states:
It is important to note potential factors driving a young person’s gender-related experience and report of gender incongruence, when carried out in the context of supporting an adolescent with self-discovery, is not considered reparative therapy as long as there is no a priori goal to change or promote one particular gender identity or expression. (p. 53)
First, the lack of an explicit, documented goal to “change or promote one particular gender identity or expression” by a psychotherapist is a scant fig leaf of protection from covert punishment of gender diversity. Second, “self-discovery” that is “supported” by compulsory psychotherapy for TGD children and adolescents is not the same as self-initiated and self-led discovery or exploration by TGD children and adolescents. Words and clarity matter.
For TGD children living and thriving in authentic, congruent gender roles, Statement 7.13 in the Children chapter is especially unsettling:
We recommend health care professionals and parents/caregivers support children to continue to explore their gender throughout the pre-pubescent years, regardless of social transition. (p. 76)
This statement implies compulsory “gender exploration” psychotherapy for all TGD youth, throughout prepubescent childhood. It presumes unfounded stereotypes of psychopathology and gaslights the gender identities of TGD children. For those who are long-established and well-adjusted in their authentic social gender roles, continual interrogation of their gender identities by a psychotherapist in a position of power and authority can be punishing.
Fortunately, Statement 7.13 is refuted within its own supporting text:
…not all gender diverse children wish to explore their gender. Cisgender children are not expected to undertake this exploration, and therefore attempts to force this with a gender diverse child, if not indicated or welcomed, can be experienced as pathologizing, intrusive and/or cisnormative.
In Summary, the principle of depsychopathologization of gender diversity is a settled principle of ethical medical practice and is no longer a legitimate topic of debate. It is frequently restated and endorsed within the SOC8 (Table 1). Yet other statements and text of the SOC8 continue to relitigate this fundamental WPATH principle. These exemplify conflict and lack of consensus within WPATH and the SOC8 authors that perpetuate false stereotypes and barriers to affirming medical treatments (Table 2).
As a consequence, contradictions to the depsychopathologization principle in the SOC8 will be harvested and weaponized by those opposed to TGD health care. Trans and Gender Diverse people needing care, along with their affirming providers, will face additional barriers from governments and health systems.
I urge the WPATH leadership to place its highest priority on a corrected SOC8.1 point-revision, that resolves these shortcomings with consistent, unambiguous cogency on the depsychopathologization of human gender diversity and access to medically necessary affirming care.
Acknowledgments
I am grateful to Dr. Antonia D’orsay and members of the International Transgender Health Forum (www.facebook.com/groups/transgenderhealth) for their extensive, collaborative analysis and dialogue on the WPATH SOC8. I also thank Attorney Lisa Gilinger for her support that made this work possible.
Copyright © 2022 Kelley Winters
References
American Academy of Family Physicians. (2012) Resolution No. 1004: Transgender Care. May 3. https://www.aafp.org/dam/AAFP/documents/about_us/special_constituencies/2012RCAR_Advocacy.pdf
American Medical Association. (2008) Resolution 122: Removing Financial Barriers to Care for Transgender Patients. https://web.archive.org/web/20120412224003/http://www.ama-assn.org/ama1/pub/upload/mm/16/a08_hod_resolutions.pdf
American Medical Association. (2022) Removing Financial Barriers to Care for Transgender Patients H-185.950. https://policysearch.ama-assn.org/policyfinder/detail/H-185.950%20Removing, https://www.sciencedirect.com/science/article/abs/pii/S2352552520300062 %20Financial%20Barriers%20to%20Care%20for%20Transgender%20Patients?uri=%2FAMADoc%2FHOD.xml-0-1128.xml
APA: American Psychiatric Association. (2010) Rationale for Proposed Revisions to P 01 Gender Dysphoria in Adolescents or Adults. DSM-5 Development, Feb. https://web.archive.org/web/20110512001831/http://www.dsm5.org/ProposedRevision/Pages/proposedrevision.aspx?rid=482#
APA: American Psychiatric Association. (2012) Position Statement on Access to Care for Transgender and Gender Variant Individuals. Aug 16. Archived: http://www.psychiatry.org/File%20Library/Advocacy%20and%20Newsroom/Position%20Statements/ps2012_TransgenderCare.pdf
APA: American Psychiatric Association. (2013A) Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Washington, D.C.: American Psychiatric Association Publishing. https://dsm.psychiatryonline.org/doi/book/10.1176/appi.books.9780890425596
APA: American Psychiatric Association. (2013B) Gender Dysphoria. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/DSM/APA_DSM-5-Gender-Dysphoria.pdf
APA: American Psychiatric Association. (2018) Position Statement on Access to Care for Transgender and Gender Variant Individuals. July. https://www.psychiatry.org/about-apa/Policy-Finder/Position-Statement-on-Access-to-Care-for-Transgend;
https://www.psychiatry.org/File%20Library/About-APA/Organization-Documents-Policies/Policies/Position-2018-Access-to-Care-for-Transgender-and-Gender-Diverse-Individuals.pdf
APA: American Psychiatric Association. (2020) Position Statement on Treatment of Transgender (Trans) and Gender Diverse Youth. July. https://www.psychiatry.org/about-apa/Policy-Finder/Position-Statement-on-Treatment-of-Transgender-(Tr
APA: American Psychiatric Association. (2022) Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition, Text Revision, DSM-5-TR. Washington, D.C.: American Psychiatric Association Publishing. https://dsm.psychiatryonline.org/doi/book/10.1176/appi.books.9780890425787
APA: American Psychiatric Association. (2022B) Gender Dysphoria. https://www.psychiatry.org/File%20Library/Psychiatrists/Practice/DSM/DSM-5-TR/APA-DSM5TR-GenderDysphoria.pdf
American Psychological Association, “Resolution on Transgender and Gender Identity and Gender Expression Non-Discrimination,” 2008, https://www.apa.org/about/policy/resolution-gender-identity.pdf
American Psychological Association. (2009) Report of the APA Task Force on Gender Identity and Gender Variance. Washington, DC., Revised, August 2019. https://www.apa.org/pi/lgbt/resources/policy/gender-identity-report.pdf
American Psychological Association. (2015) Guidelines for Psychological Practice with Transgender and Gender Nonconforming People. American Psychologist, Vol. 70, No. 9, 832– 864, December. https://www.apa.org/practice/guidelines/transgender.pdf
Ashley, F. and Baril, A. (2018). “Why ‘rapid-onset gender dysphoria’ is bad science,” The Conversation, Mar 22, https://theconversation.com/why-rapid-onset-gender-dysphoria-is-bad-science-92742
Ashley, F. (2019). Gatekeeping hormone replacement therapy for transgender patients is dehumanising. Journal of Medical Ethics, 45(7), 480–482. https://doi.org/10.1136/medethics-2018-105293)
Ashley, F. (2020). A critical commentary on ‘rapid-onset gender dysphoria.’ The Sociological Review Monographs, Vol. 68(4) 779 –79. https://www.florenceashley.com/uploads/1/2/4/4/124439164/ashley_a_critical_commentary_on_rapid-onset_gender_dysphoria.pdf
Drescher J., Cohen-Kettenis P., Winter S. (2012) Minding the body: situating gender identity diagnoses in the ICD-11. Int Rev Psychiatry. Dec;24(6):568-77. doi: 10.3109/09540261.2012.741575. PMID: 23244612.
Fisk, N. (1973). Gender dysphoria syndrome. (The how, what, and why of a disease). In D. Laub & P. Gandy (Eds.), Proceedings of the second interdisciplinary symposium on gender dysphoria syndrome (pp. 7–14). Palo Alto, CA: Stanford University Press.
Harry Benjamin International Gender Dysphoria Association. (1979) Standards of Care: The hormonal and surgical sex reassignment of gender dysphoric persons. February 12.
Harry Benjamin International Gender Dysphoria Association. (1998) The Standards of Care for Gender Identity Disorders, Fifth Edition. Düsseldorf: Symposion Publishing, June 15.
Harry Benjamin International Gender Dysphoria Association. (2005) The Standards of Care for Gender Identity Disorders, SixthVersion. Edgar, WI. [also cited in: International Journal of Transgenderism, Volume 5(1), and Journal of Psychology and Human Sexuality, (2001), Volume 13 (1), p.1‐30]
Lev, A.I., Winters, K., Alie, L., Ansara, Y., Deutsch, M., Dickey, L., Ehrbar, R., Ehrensaft, D., Green, J., Meier, S., Richmond, K., Samons, S., Susset, F., (2010). “Response to Proposed DSM-5 Diagnostic Criteria. Professionals Concerned With Gender Diagnoses in the DSM.” Retrieved May 30, 2010 from: https://web.archive.org/web/20100503030831/http://gidconcern.wordpress.com/biographies/
MacKinnon, K., Ashley, F., Kia, H., Lam, J., Krakowsky, Y., Ross, L. (2021) Preventing transition “regret”: An institutional ethnography of gender-affirming medical care assessment practices in Canada. Social Science & Medicine, 291 114477. https://doi.org/10.1016/j.socscimed.2021.114477
Olson, KR, Durwood L, Horton R, Gallagher NM, Devor A. (2022) Gender identity 5 years after social transition. Pediatrics. doi: 10.1542/peds.2021-056082
Restar, A.J. (2019). Methodological Critique of Littman’s (2018) Parental-Respondents Accounts of “Rapid-Onset Gender Dysphoria.” Arch Sex Behav 49, 61–66. https://doi.org/10.1007/s10508-019-1453-2, https://link.springer.com/article/10.1007/s10508-019-1453-2
Serano, J. (2018). Everything You Need to Know About Rapid Onset Gender Dysphoria. Medium, Aug. 22, https://juliaserano.medium.com/everything-you-need-to-know-about-rapid-onset-gender-dysphoria-1940b8afdeba
Winter, S., Diamond, M., Green, J., Karasic, D.H., Reed, T., Whittle, S., & Wylie, K.R. (2016). Transgender people: health at the margins of society. The Lancet, 388, 390-400. https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(16)00683-8/fulltext
Winters, K. (2005). Gender dissonance: Diagnostic reform of gender identity disorder for adults. Journal of Psychology and Human Sexuality, 17, 71-89.
Winters, K. (2008). Gender Madness in American Psychiatry: Essays From the Struggle for Dignity. GID Reform Advocates. Dillon, CO. https://www.amazon.com/Gender-Madness-American-Psychiatry-Struggle/dp/1439223882
Winters, K. (2011). The Proposed Gender Dysphoria Diagnosis in the DSM-5. GID Reform Weblog, June 7. https://gidreform.wordpress.com/2011/06/07/the-proposed-gender-dysphoria-diagnosis-in-the-dsm-5/
Winters, K. (2011A) New Standards of Care for the Health of Transsexual, Transgender, and Gender Nonconforming People. GID Reform Weblog, Sep 25. https://gidreform.wordpress.com/2011/09/25/new-standards-of-care-for-the-health-of-transsexual-transgender-and-gender-nonconforming-people/
Winters, K. (2013). The Proposed Gender Dysphoria Diagnosis in the DSM-5. GID Reform Weblog, June 13. https://gidreform.wordpress.com/2013/06/13/gid-reform-in-the-dsm-5-and-icd-11-a-status-update/
Winters, K. (2018). What’s Needed in the WPATH SOC8, Part 1: A Wish for Wings that Work. Trans Policy Reform Blog, Sep 26. https://transpolicyreform.wordpress.com/2018/09/26/whats-needed-in-the-wpath-soc8-part-1-a-wish-for-wings-that-work/
Winters, K. (2018B). What’s Needed in the WPATH SOC8, Part 2: A Cogent Definition of Gender Dysphoria. Trans Policy Reform Blog, Nov 7. https://transpolicyreform.wordpress.com/2018/11/07/a-wish-for-wings-that-work-part-2-a-cogent-definition-of-gender-dysphoria-for-the-soc8/
Winters, K. (2022). Transgender Affirmation in Retrograde: Historical Context for the Littmanian “ROGD” Media Blitz, Trans Policy Reform Blog. Jan 08. https://transpolicyreform.wordpress.com/2021/11/29/transgender-affirmation-in-retrograde-historical-context-for-the-littmanian-rogd-media-blitz/
Winters, K. (2022B). From the Jurassic Clarke to the SOC8: Repsychopathologization of Trans Youth, Trans Policy Reform Blog. Jan 11. https://transpolicyreform.wordpress.com/2022/01/11/from-the-jurassic-clarke-to-the-soc8-repsychopathologization-of-trans-youth/
WHO: World Health Organization. (2019). ICD-11: International classification of diseases (11th revision). https://icd.who.int/
World Professional Association for Transgender Health. (2008) WPATH Clarification on Medical Necessity of Treatment, Sex Reassignment, and Insurance Coverage in the U.S.A. June 17.
https://web.archive.org/web/20101130201438/http://wpath.org/publications_public_policy.cfm
World Professional Association for Transgender Health. (2009) WPATH Responds to Alberta, Canada’s Decision to Delist Sexual Reassignment Surgery as a Covered Medical Benefit. Apr 2021. https://amo_hub_content.s3.amazonaws.com/Association140/files
World Professional Association for Transgender Health. (2010) WPATH De-Psychopathologisation Statement. May 26. https://www.wpath.org/policies
World Professional Association for Transgender Health. (2010B) WPATH Reaction to DSM-V Criteria for Gender Incongruence, May 25. https://amo_hub_content.s3.amazonaws.com/Association140/files/WPATH%20Reaction%20to%20the%20proposed%20DSM%20-%20Final.pdf
World Professional Association for Transgender Health. (2011A) WPATH Clarification on Medical Necessity of Treatment, Sex Reassignment, and Insurance Coverage for Transgender and Transsexual People Worldwide. Captured 2011Feb05. https://web.archive.org/web/20110205134357/http://www.wpath.org/medical_necessity_statement.cfm
*World Professional Association for Transgender Health (2011B). Standards of care for the health of transsexual, transgender, and gender-nonconforming people, Version 7. https://wpath.org
World Professional Association for Transgender Health. (2014). WPATH Statement Concerning Cross-dressing, Gender-Nonconformity, and Gender Dysphoria, July 15. https://amo_hub_content.s3.amazonaws.com/Association140/files/WPATH%20Statement%20Concerning%20Cross-dressing_15%20July%202014.pdf
World Professional Association for Transgender Health. (2016). Position Statement on Medical Necessity of Treatment, Sex Reassignment, and Insurance Coverage in the U.S.A. December 21.
https://www.wpath.org/media/cms/Documents/Web%20Transfer/Policies/WPATH-Position-on-Medical-Necessity-12-21-2016.pdf
World Professional Association for Transgender Health. (2016B). Language and Trans Health, Dec. 15. [also cited, Bouman, Schwend, et al. (2016) Language and trans health, International Journal of Transgenderism, 18:1, 1-6, DOI: 10.1080/15532739.2016.1262127] https://www.wpath.org/media/cms/Documents/Resources/Language%20Policy.pdf
World Professional Association for Transgender Health (2016C). WPATH 24th Scientific Symposium, Program Announcement, June 17-21. Amsterdam. Captured 2016: http://wpath2016.conferencespot.org/62620-wpathv2-1.3138789/t002-1.3139895/f0240-1.3140049/0706-000039-1.3140052
World Professional Association for Transgender Health. (2017). Letter to Roger Severino, U.S. Department of Health and Human Services. Aug 15. https://wpath.org/policies
World Professional Association for Transgender Health. (2018). WPATH position on “Rapid Onset Gender Dysphoria (ROGD).” https://www.wpath.org/media/cms/Documents/Public%20Policies/2018/9_Sept/WPATH%20Position%20on%20Rapid-Onset%20Gender%20Dysphoria_9-4-2018.pdf
World Professional Association for Transgender Health. (2019). WPATH Board Responds to Health Care Policies and Practices Imposed by Certain Religious Institutions. May 17. https://wpath.org/media/cms/Documents/Public%20Policies/2019/5-16_Religious%20Institution%20Health%20Policies.pdf
World Professional Association for Transgender Health, et al. (2019B) WPATH, USPATH, EPATH Statement in Response to Calls for Banning Evidence-Based Supportive Health Interventions for Transgender and Gender-Diverse Youth. Nov. 22. [also cited, Leibowitz, S., Green, J. et al. (2020) Statement in response to calls for banning evidence-based supportive health interventions for transgender and gender diverse youth, International Journal of Transgender Health, 21:1, 111-112, DOI: 10.1080/15532739.2020.1703652]
https://www.wpath.org/media/cms/Documents/Public%20Policies/2019/FINAL%20Statement%20in%20Response%20to%20Calls%20for%20Banning%20Evidence-Based%20Supportive%20Health%20Interventions%20for%20Transgender%20and%20Gender-Diverse%20Youth%2011-20-2019.pdf
World Professional Association for Transgender Health. (2020A) WPATH / USPATH Statement on Resumption of Gender-Affirming Surgery During COVID-19 Pandemic. May 8. https://wpath.org/media/cms/Documents/Public%20Policies/2020/FINAL%20Joint%20WPATH%20USPATH%20Statement%20On%20Resumption%20of%20Medically%20Necessary%20Surgeries%20During%20COVID.pdf
World Professional Association for Transgender Health. (2020B) WPATH Sends Letter of Support to Republic of Kazakhstan. July 1. https://wpath.org/media/cms/Documents/Public%20Policies/2020/Republic%20of%20Kazakhstan%20-%20Letter%20of%20Support%20July%201%202020.pdf
World Professional Association for Transgender Health. (2021) Bell v Tavistock and Portman NHS Foundation Trust [2020] EWHC 3274: Weighing current knowledge and uncertainties in decisions about gender-related treatment for transgender adolescents. Apr 5. [Also cited as: de Vries, et al. (2021) Bell v Tavistock and Portman NHS Foundation Trust [2020] EWHC 3274: Weighing current knowledge and uncertainties in decisions about gender-related treatment for transgender adolescents. International Journal of Transgender Health, DOI: 10.1080/26895269.2021.1904330]
https://www.wpath.org/media/cms/Documents/Public%20Policies/2021/Bell%20v%20Tavistock%20and%20Portman%20NHS%20Foundation%20Trust%202020%20EWHC%203274%20Weighing%20current%20knowledge%20and%20uncertainties%20in%20decisions%20about.pdf
*World Professional Association for Transgender Health (2022). Standards of Care for the Health of Transgender and Gender Diverse People, Version 8. https://wpath.org
* Revisions of WPATH Standards of Care were traditionally published twice, on the WPATH (formerly HBIGDA) web site and in behavioral journals, including the Journal of Psychology & Human Sexuality, International Journal of Transgenderism, and, most recently, International Journal of Transgender Health. For brevity and accessibility, SOC documents published directly by WPATH are referenced here.
References with Content Warning
The following references contain material that in the author’s opinion may be ideologically biased, in opposition to affirming medical care, civil rights, equality, or participation in human society for Transgender and Gender Diverse people. This content may trigger trauma in TGD readers or those who care about TGD lives.
Alliance Defending Freedom. (2022). Gender Dysphoria Expert Discusses the Science Regarding Gender Identity. https://adflegal.org/article/gender-dysphoria-expert-discusses-science-regarding-gender-identity
Littman, L. (2018). Rapid-onset gender dysphoria in adolescents and young adults: A study of parental reports. PLOS ONE 13(8): e0202330. doi.org/10.1371/journal.pone.0202330
Littman, L. (2021). Individuals treated for gender dysphoria with medical and/or surgical transition who subsequently detransitioned: A survey of 100 detransitioners. Archives of Sexual Behavior, 50(8), 3353–3369. https://doi.org/10.1007/s10508-021-02163-w.
Zucker, K. (2016). The Clinical Practitioner’s Perspective. World Professional Association for Transgender Health 24th Scientific Symposium, June 20. Amsterdam.

